The Red Meat Allergy: A Canadian Perspective
This guest post is written by Shaun Dergousoff, PhD, a research scientist at AAFC Lethbridge focused on tick populations and arthropod vectors of livestock disease. The following is an updated version of an article we first published on the BCRC Blog in 2017.
Recently, a connection between the bite of the lone star tick and allergies to red meat products was established. The “red meat allergy” is often framed as an emerging and alarming public health issue. Although the allergy symptoms can be severe, the incidence is relatively low, even throughout the southeastern United States where the lone star tick is well established (meaning a presence of reproducing populations).
The red meat allergy was first identified in Australia with several hundred cases diagnosed since 1985, and was recognized in thousands of people in the southeastern United States over the last couple decades. This allergy also occurs in people from several other countries around the world. Based on reported cases, it appears that allergy to red meat in the USA is about as common as allergy to peanuts, occurring in only 0.1% of the population. Those who are affected can have very serious and even life-threatening anaphylactic reactions after eating red meat products.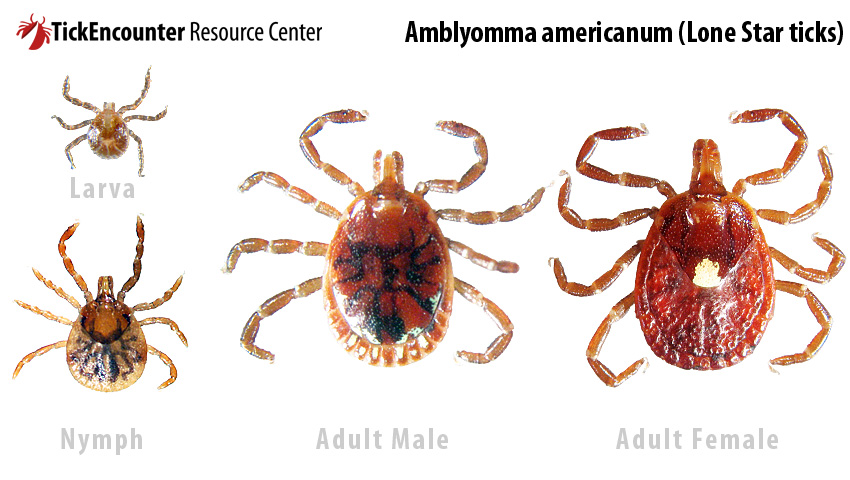
The source of the red meat allergy was a mystery until 2007 when doctors realized that a large proportion of the people that were diagnosed also reported tick bites weeks or months prior to experiencing symptoms.
When a tick attaches to a person or animal (“host”), it will feed on blood for several days if not removed. During this time it injects saliva directly into the host’s bloodstream. Ticks have a few tricks up their sleeves and some of the salivary compounds act as an anaesthetic so the host cannot feel the tick bite. Other compounds injected by the tick alter the host’s immune response. Susceptible people produce antibodies to carbohydrates (sugars) in the tick’s saliva that are different than the types of carbohydrates found our bodies. One to three months after being exposed to the tick, the host’s primed immune system can produce antibodies to a similar carbohydrate called galactose-alpha-1,3-galactose, more commonly called alpha-gal, which is found in cells of non-primate mammals. The production of antibodies to alpha-gal can lead to allergic reactions in people (“alpha-gal syndrome”).
The allergic reaction occurs 2 to 10 hours after eating red meat (beef, pork, and lamb, but not chicken or fish), or other animal products, such as gelatin and milk. This is generally much longer delay than most allergic reactions, which are typically more immediate. Symptoms can be relatively mild with hives and swelling but can also end up as a severe anaphylactic reaction that requires a shot of epinephrine. To confirm that the allergy is to red meat, doctors use a test that detects antibodies to alpha-gal. For some people, the reaction can become less severe or even be eliminated over time if they prevent further exposure to tick bites.
Almost all cases of alpha-gal syndrome in the USA occur in areas where the lone star tick is present. None of the tick species that are currently established in Canada appear to cause the allergy.
The increase in the number of red meat allergy cases, which spurred the recent media reports, may be partly due to changes in lone star tick populations. In some regions the ticks are becoming more abundant. They are also spreading into new areas, with increasing reports of individual ticks and established populations the in northeastern states, including Michigan, Minnesota and New York. So, it’s likely that the tick will continue to move northward, but this would be limited by the availability of suitable habitat for tick development and survival. A recent study1 predicts that the most southern parts of Ontario and Nova Scotia may have suitable habitat to support lone star tick populations in the next few decades.
It is important to also be aware of the lone star tick because it actively seeks out hosts and can also transmit a long list of human and animal pathogens, including those that cause serious diseases, such as Heartland virus disease, Bourbon virus disease, southern tick-associated rash illness, ehrlichiosis, rickettsiosis, tularemia, and theileriosis. Fortunately, these pathogens are relatively rare and the bacteria that causes Lyme disease cannot be transmitted by the lone star tick.
Several provincial and national surveillance programs are monitoring the presence of ticks in Canada. Lone star ticks are generally collected in Alberta, British Columbia, Manitoba, Newfoundland, Nova Scotia, Quebec, and more commonly in Ontario; the majority are from people or dogs that spent time in areas of the USA where this tick normally occurs. Occasionally, single lone star ticks are collected directly from the vegetation, or from animals or people. These ticks most likely hitched a ride on migrating birds and fell off a few days after attaching.
There still is no evidence that the lone star tick has become established in Canada, and it is only occasionally reported on animals or people. This difference between reported occurrences of a tick and establishment of a population is very important when considering the level of risk to people and how to manage it.
So, what does the “red meat allergy” mean for the Canadian public and beef industry? Currently, the chance of encountering a lone star tick is extremely low. Also, a relatively small proportion of the human population is susceptible to developing an allergy to red meat and few ticks are infected with pathogens. Awareness and tick bite prevention continue to be the most important steps to take in response to ticks while enjoying the great outdoors.
Learn More
- For more information and images of the lone star tick see the Tick Encounter website: http://www.tickencounter.org/tick_identification/lone_star_tick
- For information on prevention of tick (and mosquito) bites, refer to this article from the Canadian Paediatric Society: http://www.cps.ca/en/documents/position/preventing-mosquito-and-tick-bites
- The American College of Allergy, Asthma & Immunology has more information on the red meat allergy: http://acaai.org/allergies/types/food-allergies/types-food-allergy/meat-allergy
References
- Raghavan, R. K., A. T. Peterson, M. E. Cobos, R. Ganta, and D. Foley. 2019. Current and Future Distribution of the Lone Star Tick, Amblyomma americanum (L.) (Acari: Ixodidae) in North America. PLOS ONE. 14: e0209082.
Click here to subscribe to the BCRC Blog and receive email notifications when new content is posted.
The sharing or reprinting of BCRC Blog articles is welcome and encouraged. Please provide acknowledgement to the Beef Cattle Research Council, list the website address, www.BeefResearch.ca, and let us know you chose to share the article by emailing us at [email protected].
We welcome your questions, comments and suggestions. Contact us directly or generate public discussion by posting your thoughts below.